You Need the Bugs in Your Mouth! They Can Even Help Lower Your Blood Pressure
Jacqueline Carcaramo, BSDH, RDH
The Oral-Systemic Connection
For decades, we’ve been told to brush and floss twice daily for a healthy mouth. Yet, often, people still don’t fully understand the importance of oral health and its impact on the rest of the body. The oral-systemic connection is well-researched, and poor oral health can contribute to a range of severe conditions including diabetes, arthritis, obesity, cardiovascular disease, pregnancy complications, and even Alzheimer’s disease. (1) Keeping the oral microbiome in balance is key to maintaining good oral and overall health.
What is the oral microbiome and why does it matter?
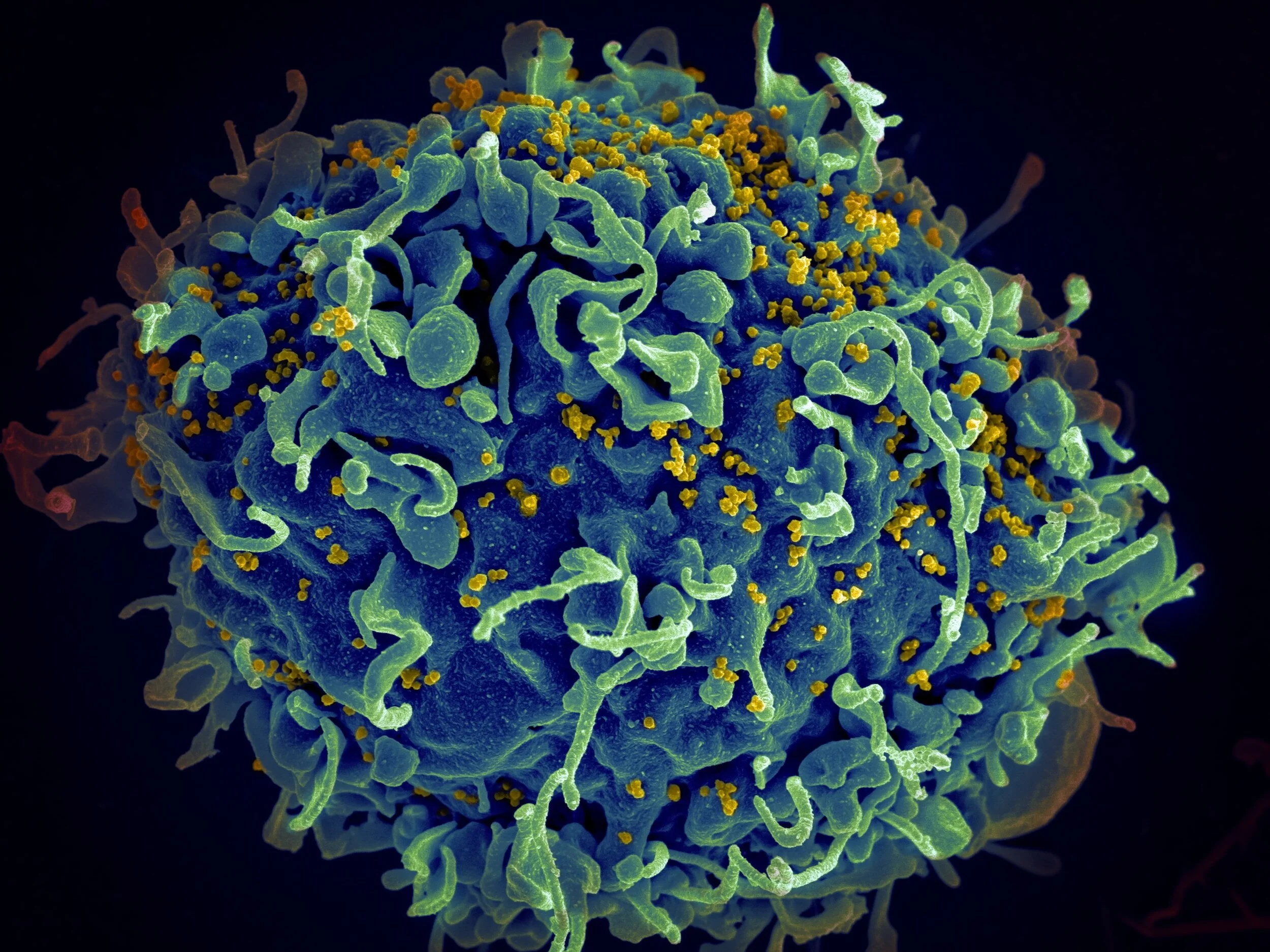
The term microbiome refers to the accumulation of microorganisms (bacteria, fungi, protozoa) in a specific environment. Just like the gut microbiome, the oral microbiome plays a powerful role in our overall health. In a healthy mouth, these microorganisms are diverse and well-balanced. Disruptions to this balance can lead to oral dysbiosis, where harmful bacteria take over and can wreak havoc. Oral dysbiosis can stimulate or progress gingivitis, periodontal disease, cavities, and even oral cancer.
Recent research has debated how certain antiseptic mouthwashes, commonly used in households to eliminate harmful oral bacteria, may also destroy beneficial bacteria. Some of these bacteria help to generate nitric oxide (NO). Nitric oxide is a necessary signaling molecule that regulates not only oral health, but also systemic blood flow, the immune system, and neurotransmission.
Why is good oral health important for nitric oxide production?
The human body naturally produces nitric oxide through good endothelial function. The endothelium, which is the thin lining of the blood vessels, regulates blood flow by producing nitric oxide. Various factors can impact endothelial function like age, exercise, genetics, and lifestyle habits. Nitric oxide is a vasodilator, meaning it helps to open the blood vessels and adjusts blood flow. Along with the endothelium, nitric oxide can also be generated through the nasal mucosa and sinuses.
When we breathe through our noses, we are able to move this nitric oxide to our lungs. This helps to filter out some potentially harmful contaminants in the air through nitric oxide’s antibacterial capabilities and also creates a consistently superior airflow. Individuals that chronically mouth breathe are missing out on this route of nitric oxide uptake.
If you have poor endothelial function and chronically mouth breathe, you probably have very little nitric oxide unless you’re getting it through your diet. Yes, nitric oxide can be developed through diet too. The healthiest form of dietary nitrates comes from vegetables. When we eat nitrate-rich veggies like beets or lettuce, the nitrates in these foods move through the GI tract and are absorbed into the blood. About 75% of the nitrates are excreted into the kidneys and 25% move to the salivary glands. (2) Once the nitrates are flooded into the mouth through saliva, specific nitrate-reducing oral bacteria change nitrate into its modified form, nitrite. Nitrite is continually swallowed and moves through the digestive system, where it is transformed into nitric oxide. This route of nitric oxide development relies on the presence of nitrate-reducing bacteria in the mouth. Keeping your oral microbiome well-balanced can lead to considerable health benefits. Those helpful little nitrate-reducing bacteria can be wiped out with something as seemingly harmless as your daily swish of antiseptic mouthwash.
Does mouthwash ruin your oral microbiome?
Antiseptic mouthwash has had a mixed reputation. We want to rid ourselves of disease and we know that antiseptics kill the bad bugs, but we also know that too much of anything isn’t good. The issue at hand is that antiseptics indiscriminately kill bacteria, whether they are helpful or harmful to us.
Eliminating most of your oral bacteria through repetitive use of an antiseptic mouthwash can create a major shift in the mouth, called oral dysbiosis. This imbalance leaves room for any lingering disease-causing bacteria to multiply and take over. Working toward homeostasis in the mouth is the optimal approach to reducing the risk of cavities and gum disease. A mouth with less nitrate-reducing bacteria and more disease-causing bacteria correlates with chronic gum disease and later, cardiovascular disease. (3)
Interestingly, your oral health can be directly impacted by incorporating dietary nitrates. Researchers have found salivary nitrate decreases cavity risk and gum inflammation. (4) Salivary nitrate even helps the oral microbiome thrive by improving the conditions for helpful oral microbes and removing cavity-causing and inflammatory microbes. By using an antiseptic mouthwash, however, this balance in the oral environment is disrupted.
Antiseptic mouthwash has been shown to reduce the oral environment’s ability to reduce dietary nitrates into nitrites, which later transform into nitric oxide. (5) Using antiseptic mouthwash can actually increase blood pressure because it reduces the production of nitric oxide. Therefore, there is a correlation between the use of antiseptic mouthwash and the decrease in nitric oxide production, which can lead to an increase in blood pressure. (6)
With heart disease being the leading cause of death in the United States, and knowledge that disruption of the oral microbiome can increase blood pressure, this topic should be regularly discussed with the general public. Therefore, something as simple as the choice of mouthwash can contribute to something as crucial as heart health.
So what qualifies as antiseptic mouthwash and should we ever use it again?
You may be thinking, is alcohol-based mouthwash a culprit too? It’s best to avoid consistent use of alcohol-based mouthwashes as alcohol has cytotoxic effects on bacteria. (7) They can also dry out the mouth if used long-term. That’s the key term here, long-term or chronic use. Using an antiseptic or alcohol-based mouthwash once in a while to clear up an infection isn’t going to cause catastrophic changes. It will briefly alter your oral microbiome, but if you allow it to bounce back to its thriving self, it shouldn’t cause too much distress. It’s the constant use of these mouthwashes that can cause more trouble.
It’s like regularly taking antibiotics, which deplete the harmful and the beneficial bacteria in your gut and can bring about other health issues. It’s why you hear people recommending probiotics when using antibiotics because destroying everything causes dysbiosis. Even “bad” bacteria can be left alone if they aren’t triggered by external factors that cause them to act out in devilish ways.
Think of your mouth as a garden. By properly caring for the plants (bacteria and other microbes), the garden grows rich. If you’re treating the garden with things that will make it weak and not properly caring for it, the garden will be destroyed. In the end, nix the mouthwash. If you have a mouth sore or bleeding gums, work on better oral hygiene and swish with some warm salt water. (8)
Don’t cover up the issue with a minty quick fix.
Maintaining good oral hygiene habits such as daily brushing, flossing, and tongue cleaning is essential for keeping your mouth healthy and your oral microbes in check. Tongue cleaning, in particular, can help prevent the buildup of substances that cause bad breath. While bad breath can be caused by an imbalanced oral microbiome or underlying health condition, using antiseptic mouthwash as a temporary solution is not a viable long-term solution. Instead, focusing on a nourishing diet and consuming pre and probiotic-rich foods can help restore harmony to the oral microbiome and promote overall health. Prioritizing excellent oral hygiene, breathing through your nose, and adopting a balanced diet can help maintain the natural stability of your mouth's microbes and keep your blood pressure under control.
References
1. Kapila YL. Oral health’s inextricable connection to systemic health: Special populations bring to bear multimodal relationships and factors connecting periodontal disease to systemic diseases and conditions. Periodontol 2000. 2021 Oct;87(1):11–6.
2. Hezel MP, Weitzberg E. The oral microbiome and nitric oxide homeostasis. Oral Dis. 2015 Jan;21(1):7–16.
3. Pignatelli P, Fabietti G, Ricci A, Piattelli A, Curia MC. How Periodontal Disease and Presence of Nitric Oxide Reducing Oral Bacteria Can Affect Blood Pressure. International Journal of Molecular Sciences. 2020 Jan;21(20):7538.
4. Rosier BT, Buetas E, Moya-Gonzalvez EM, Artacho A, Mira A. Nitrate as a potential prebiotic for the oral microbiome. Scientific Reports 2020 10:1. 2020;10(1):1–15.
5. Govoni M, Jansson EÅ, Weitzberg E, Lundberg JO. The increase in plasma nitrite after a dietary nitrate load is markedly attenuated by an antibacterial mouthwash. Nitric Oxide. 2008;19(4):333–7.
6. Bryan NS, Tribble G, Angelov N. Oral Microbiome and Nitric Oxide: the Missing Link in the Management of Blood Pressure. Current hypertension reports [Internet]. 2017;19(4). Available from: https://pubmed.ncbi.nlm.nih.gov/28353075/
7. Fan X, Peters BA, Jacobs EJ, Gapstur SM, Purdue MP, Freedman ND, et al. Drinking alcohol is associated with variation in the human oral microbiome in a large study of American adults. Microbiome. 2018;6(1):59.
8. Gupta S, Jain A, Singla M. Is saltwater mouth rinse as effective as chlorhexidine following periodontal surgery? Evid Based Dent. 2021 Dec;22(4):130–1.